Sleeve Gastrectomy vs. Gastric Bypass: Which Is Right for You?
Choosing to undergo weight loss surgery is a life-changing decision—one that goes far beyond shedding pounds. For many individuals struggling with obesity and related health issues like diabetes, high blood pressure, and sleep apnea, bariatric surgery offers a path to not only a healthier body but a fuller, more active life. Among the most commonly performed procedures worldwide are Sleeve Gastrectomy and Gastric Bypass.
Though both are effective tools for significant and sustained weight loss, they differ greatly in how they’re performed, how they affect your digestive system, and what they require in terms of long-term lifestyle changes. Understanding the unique benefits, risks, and outcomes of each can help you make an informed decision in consultation with your healthcare team.
In this blog, we’ll break down how each surgery works, compare their effectiveness and side effects, and guide you in deciding which option may be better suited to your personal health goals.
What Is Sleeve Gastrectomy?
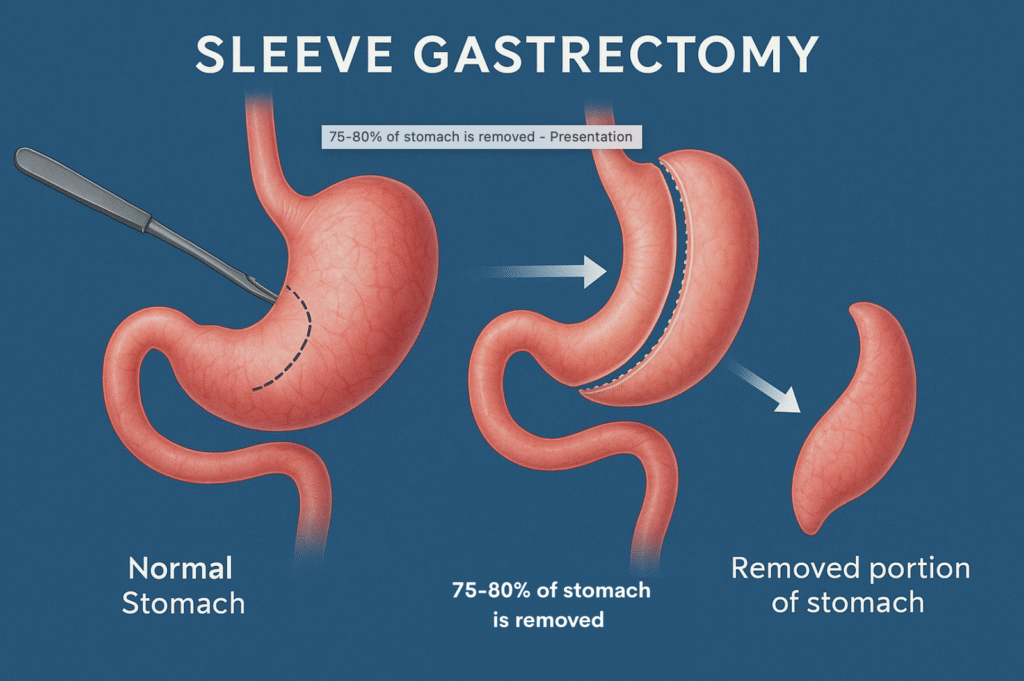
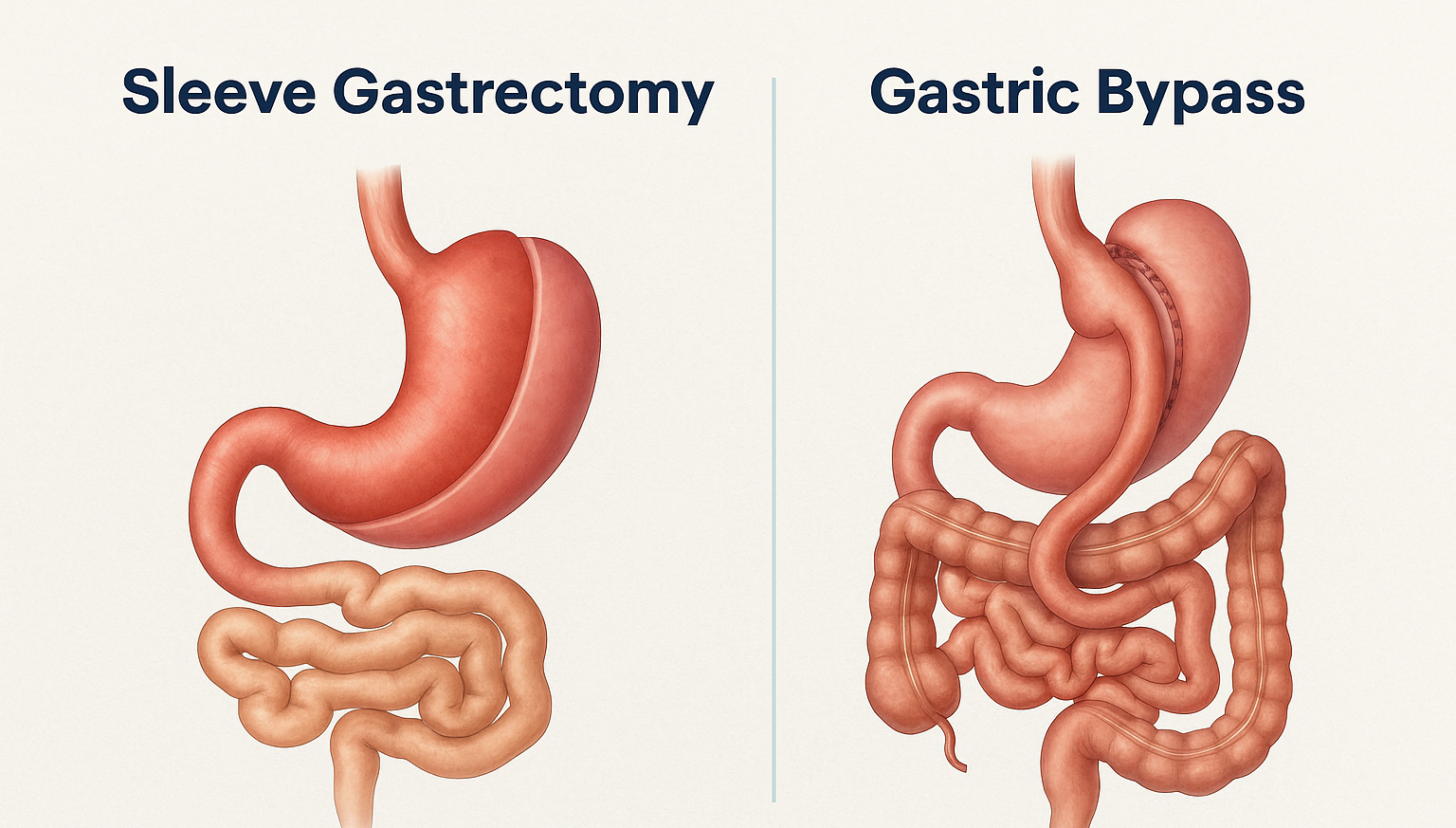
Sleeve Gastrectomy, also known as Vertical Sleeve Gastrectomy (VSG), is a restrictive weight loss surgery that significantly reduces the size of your stomach. During the procedure, the surgeon removes approximately 75–80% of the stomach, particularly the curved outer portion called the greater curvature. The remaining stomach is reshaped into a slender, banana-shaped tube—or “sleeve”—that holds much less food.
- How It Works:
The procedure doesn’t involve rerouting the intestines or changing the digestive process. Instead, it works in two main ways:
- Restricting Intake:
The new, smaller stomach can only hold around 100 to 150 mL of food (about the size of a small cup), significantly less than the original capacity. This naturally leads to reduced food intake during meals and a feeling of fullness after eating smaller portions. - Hormonal Changes:
During the surgery, the part of the stomach that produces most of the hormone ghrelin (often called the “hunger hormone”) is removed. Ghrelin stimulates appetite, so with its levels greatly reduced, patients often feel less hungry between meals, making it easier to manage cravings and reduce overall calorie intake.
- Key Features:
- Purely restrictive: No intestinal rerouting.
- Shorter operative time.
- Lower risk of nutritional deficiencies compared to bypass.
- Irreversible, as the stomach is permanently removed.
- Benefits of Sleeve Gastrectomy:
- Lower risk of complications.
- No rerouting of intestines, preserving normal digestion.
- Suitable for patients with anemia or existing nutritional deficiencies.
- Fewer long-term complications like internal hernias.
Sleeve Gastrectomy Risks:
- Not reversible.
- Potential for worsening acid reflux or GERD.
- Risk of staple line leaks and narrowing of the sleeve.
What Is Gastric Bypass?
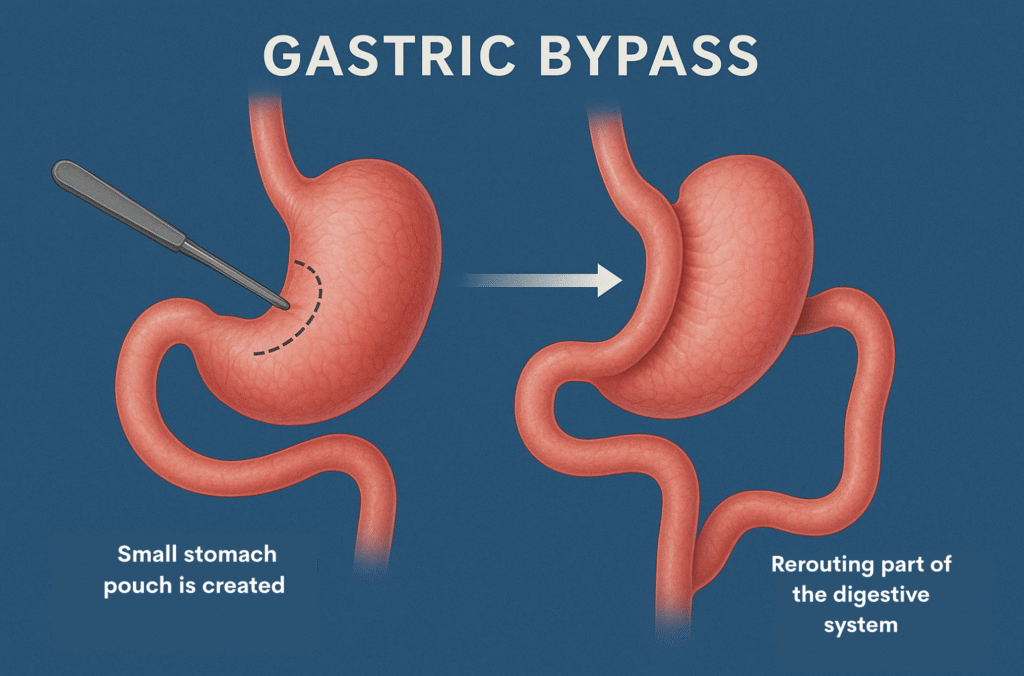
Gastric Bypass, medically known as Roux-en-Y Gastric Bypass (RYGB), is both a restrictive and malabsorptive weight loss surgery. It works by creating a small stomach pouch and rerouting part of the digestive system. This approach not only limits how much food you can eat but also reduces how many calories and nutrients your body absorbs from the food.
- How It Works:
Gastric Bypass aids in weight loss through two major mechanisms:
Restricting Intake:
During the procedure, the surgeon creates a small pouch at the top portion of the stomach—about the size of an egg. This pouch becomes the new, smaller stomach and is capable of holding only a few tablespoons of food at a time. As a result, patients feel full after eating small portions, leading to a significant reduction in daily calorie intake.
Reducing Absorption:
After creating the stomach pouch, the surgeon connects it directly to a lower part of the small intestine (called the jejunum), bypassing the rest of the stomach and the upper part of the small intestine (duodenum). Because food skips part of the digestive tract, the body absorbs fewer calories and nutrients. This contributes to faster and more significant weight loss compared to procedures that are purely restrictive.
- Key Features:
- Restrictive + malabsorptive.
- More effective in some patients with severe obesity or diabetes.
- Greater long-term weight loss potential.
- More complex surgery with higher risk of complications.
- Benefits of Sleeve Gastrectomy:
- Often more effective for severe obesity, diabetes, and metabolic syndrome.
- Better outcomes for patients with severe GERD.
- Rapid weight loss and higher total excess weight loss.
Sleeve Gastrectomy Risks:
- Higher risk of dumping syndrome, where food moves too quickly into the intestine.
- Vitamin and mineral deficiencies (iron, B12, calcium) due to bypassed intestines.
- Risk of internal hernias and intestinal obstruction.
- Requires lifelong supplementation and monitoring.
Sleeve Gastrectomy vs. Gastric Bypass: A Detailed Comparison
When considering weight loss surgery, understanding the differences between Sleeve Gastrectomy (VSG) and Gastric Bypass (Roux-en-Y or RYGB) is essential. Below is a comprehensive breakdown of how these two procedures differ across multiple key factors:
1. Surgical Complexity
Sleeve Gastrectomy is a simpler, less invasive procedure since it does not involve intestinal rerouting. Gastric Bypass is more complex as it requires reconstructing part of the digestive system.
2. Reversibility
The sleeve procedure is permanent and cannot be reversed. Gastric Bypass is technically reversible, but doing so is rare and complicated.
3. Stomach Size After Surgery
Post-surgery, the sleeve holds about 100 to 150 mL of food. The gastric bypass pouch is smaller, typically holding only 15 to 30 mL—roughly the size of an egg.
4. Food Restriction
Both procedures restrict how much food you can eat, but they do so differently. Sleeve Gastrectomy limits intake by reducing stomach volume, while Gastric Bypass restricts intake and also changes how food moves through the digestive system.
5. Malabsorption
Sleeve Gastrectomy does not affect the absorption of nutrients. In contrast, Gastric Bypass significantly reduces nutrient and calorie absorption, making it both a restrictive and malabsorptive procedure.
6. Hunger Hormones
Sleeve Gastrectomy greatly reduces levels of ghrelin, the hunger hormone, because the part of the stomach that produces it is removed. Gastric Bypass also reduces ghrelin, but to a lesser extent.
7. Expected Weight Loss
Patients typically lose 50–60% of their excess weight within one to two years with Sleeve Gastrectomy. Gastric Bypass patients often lose slightly more—around 60–70% of their excess weight over the same period.
8. Impact on Type 2 Diabetes
While both surgeries can improve or even resolve Type 2 diabetes, Gastric Bypass tends to have a greater and more immediate effect, often leading to remission even before significant weight loss occurs.
9. GERD (Gastroesophageal Reflux Disease)
Sleeve Gastrectomy may worsen or even cause GERD in some patients. In contrast, Gastric Bypass is usually effective in reducing or resolving reflux symptoms.
10. Dumping Syndrome
Dumping syndrome—a condition where food moves too quickly into the small intestine—rarely occurs with Sleeve Gastrectomy but is more common with Gastric Bypass, especially when sugary foods are consumed.
11. Nutrient Deficiency Risk
Because Gastric Bypass affects nutrient absorption, it carries a higher risk of vitamin and mineral deficiencies, particularly in B12, iron, calcium, and vitamin D. Sleeve patients also face deficiencies but to a lesser degree.
12. Hospital Stay and Recovery Time
Sleeve Gastrectomy typically requires a hospital stay of 1–2 days and a recovery period of 2–4 weeks. Gastric Bypass usually involves a slightly longer hospital stay (2–3 days) and a recovery time of 3–6 weeks.
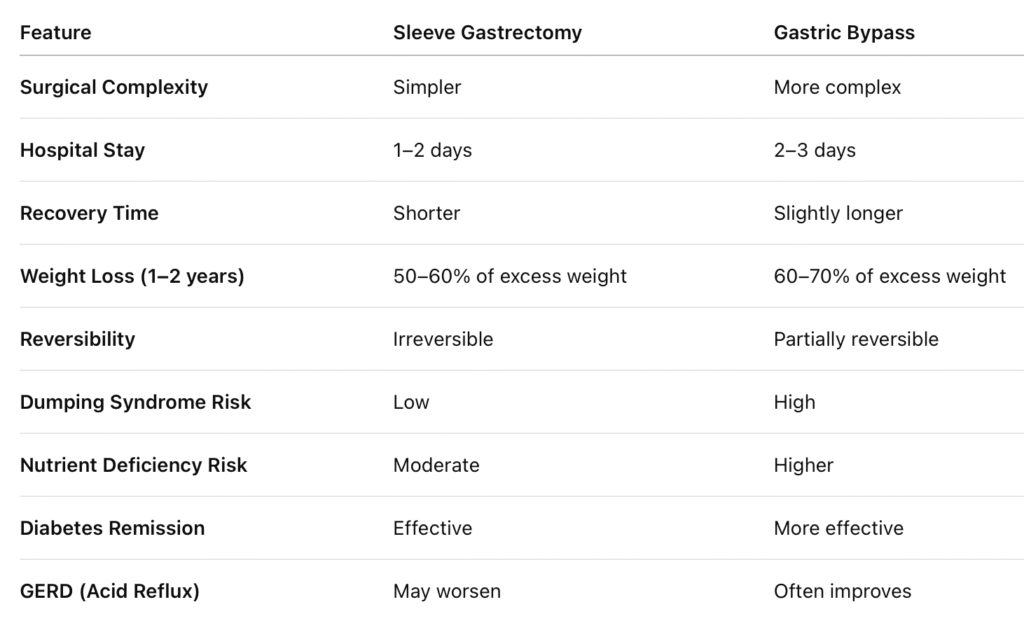
Long-Term Follow-Up
Both procedures require regular follow-up to monitor nutrition and overall health. However, because of the malabsorption involved, Gastric Bypass patients often need more intensive, lifelong monitoring and supplementation.
In Summary
Choose Sleeve Gastrectomy if you want a simpler, less invasive procedure with fewer nutritional risks, and you don’t suffer from acid reflux.
Choose Gastric Bypass if you have severe obesity, Type 2 diabetes, or bad acid reflux, and you’re okay with a more complex surgery and lifelong supplement use.
| Criteria | Sleeve Gastrectomy (VSG) | Gastric Bypass (RYGB) |
|---|---|---|
| Type of Surgery | Part of the stomach is removed (about 75–80%) | A small stomach pouch is created and connected to the small intestine, bypassing most of the stomach and some of the intestine |
| Simplicity | Simpler, less invasive | More complex, involves rerouting intestines |
| Reversibility | Not reversible | Partially reversible |
| Stomach Size After Surgery | 100–150 mL (banana-shaped sleeve) | Small pouch (15–30 mL) |
| Food Restriction | Yes (smaller stomach = less food) | Yes (small pouch + food bypasses part of the gut) |
| Malabsorption (reduced nutrient absorption) | No | Yes – nutrients and calories are absorbed less |
| Hunger Hormone Reduction (ghrelin) | Yes, significantly reduced | Yes, but less than sleeve |
| Expected Weight Loss | 50–60% of excess weight in 1–2 years | 60–70% of excess weight in 1–2 years |
| Impact on Type 2 Diabetes | Improves, especially in early cases | More effective—can cause remission |
| GERD (Acid Reflux) | May worsen or develop post-surgery | Often improves or resolves GERD |
| Dumping Syndrome Risk | Low risk | High risk—especially if sugary foods are eaten |
| Nutrient Deficiency Risk | Moderate (mainly B12, iron) | Higher—requires lifelong supplements |
| Hospital Stay | 1–2 days | 2–3 days |
| Recovery Time | 2–4 weeks | 3–6 weeks |
| Long-Term Follow-Up | Needed | Needed (more intensive due to malabsorption) |
Final Thoughts
Both Sleeve Gastrectomy and Gastric Bypass have proven to be powerful tools in the fight against obesity, offering not just weight loss but improved health, increased energy, and a better quality of life. While Sleeve Gastrectomy is simpler and primarily restrictive, Gastric Bypass offers additional benefits through its malabsorptive effects—making it especially effective for patients with severe obesity or conditions like Type 2 diabetes and acid reflux.
However, there’s no one-size-fits-all answer. Your decision should be based on your medical history, lifestyle, weight loss goals, and discussions with a qualified bariatric surgeon. With the right support and mindset, either surgery can be the start of a healthier, more empowered future. The Digestive Health Institute by Dr. Muffi provides expert consultation and resources to help guide you through your weight loss surgery journey, ensuring that you’re fully informed every step of the way.
Remember, the surgery is just the beginning—the real transformation comes with the choices you make afterward.