Types of Hysterectomy
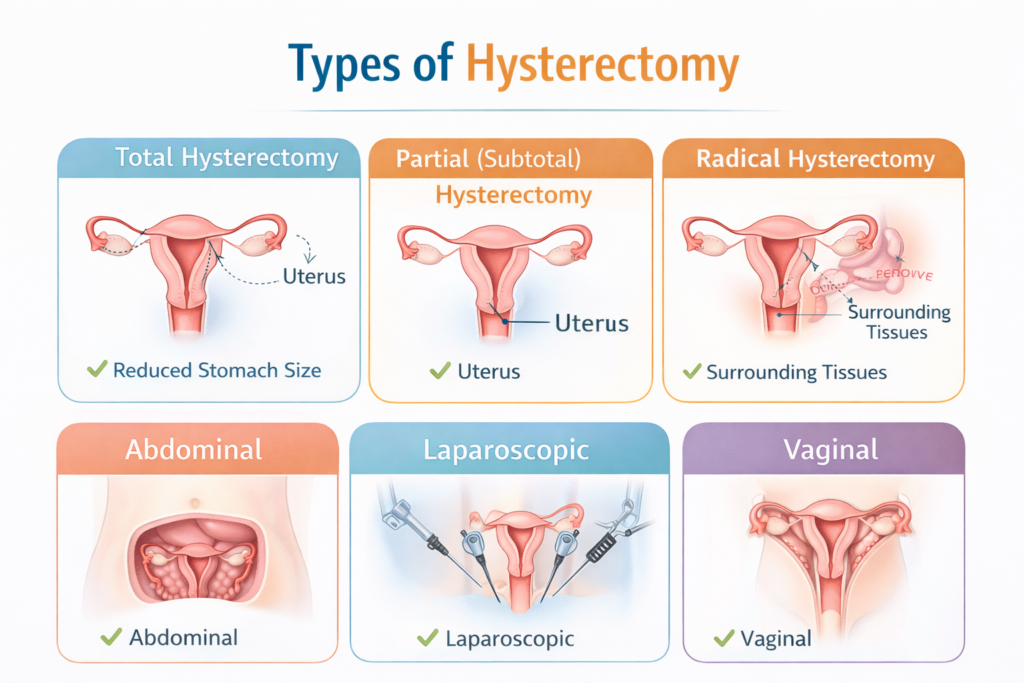
Types of Hysterectomy: Complete Guide for Patients
Hysterectomy is one of the most common surgeries performed in gynecology, yet many patients are unsure which type is right for them. Choosing the right procedure depends on your health, symptoms, age, and whether you want to preserve your ovaries. In this guide, we’ll explain all types of hysterectomy, surgical approaches, recovery, and what to expect after surgery.
What is a Hysterectomy?
A hysterectomy is a surgical procedure to remove your uterus. Depending on your condition, your surgeon may also remove:
- Cervix
- Ovaries (oophorectomy)
- Fallopian tubes (salpingectomy)
- Part of the vagina or surrounding tissues
After a hysterectomy, you will no longer get your period and cannot become pregnant. If your ovaries are removed, menopause begins immediately.
Why Do People Get a Hysterectomy?
Hysterectomies are often recommended for:
- Abnormal or heavy bleeding
- Uterine fibroids or noncancerous tumors
- Endometriosis or severe pelvic pain
- Uterine prolapse causing urinary/fecal incontinence
- Cancer (uterine, cervical, ovarian)
- High risk of cancer (preventive hysterectomy)
- Complications after childbirth, like uterine rupture
Before recommending surgery, your doctor may try medications, hormone therapy, or minimally invasive procedures.
Types of Hysterectomy by Organs Removed
Type | Organs Removed | Menopause Impact | Who It’s For |
Total Hysterectomy | Uterus + Cervix | No, if ovaries preserved | Common benign conditions |
Supracervical (Partial) Hysterectomy | Upper uterus only | No | Preserve cervix, avoid Pap changes |
Total + Bilateral Salpingo-Oophorectomy | Uterus + Cervix + Ovaries + Fallopian tubes | Yes, immediate | Cancer risk, endometriosis, severe symptoms |
Radical Hysterectomy | Uterus + Cervix + Ovaries + Fallopian tubes + upper vagina + surrounding tissue | Yes | Usually for cancer |
Surgical Variations | See below | N/A | Based on approach |
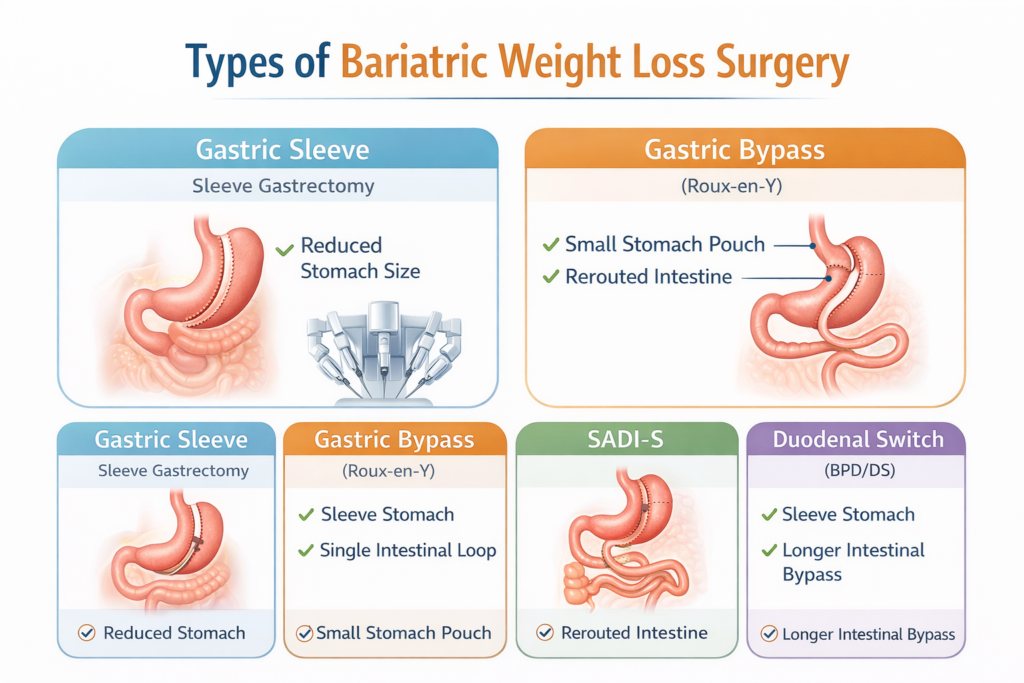
Types of Hysterectomy by Surgical Approach
1️ Vaginal Hysterectomy
- Uterus removed through the vagina
- No abdominal incision
- Shortest recovery: ~2–4 weeks
- Often outpatient surgery
- Low complication rate
2️ Laparoscopic Hysterectomy
- Small abdominal incisions with a camera and instruments
- Surgeon removes uterus in pieces through incisions or vagina
- Recovery: 2–4 weeks
- Less pain than open surgery
3️ Robotic-Assisted Laparoscopic Hysterectomy
- Surgeon uses robotic arms for precision
- Small incisions similar to laparoscopic surgery
- Recovery: ~2–4 weeks
- Advantages:
- 3D magnified view
- Better precision, less blood loss
- Ideal for complex cases, scar tissue, or large fibroids
- 3D magnified view
4️ Abdominal Hysterectomy
- Traditional open surgery via 6–8 inch incision
- Longer hospital stay (2–3 days)
- Recovery: 4–6 weeks
- Often required for:
- Large uterus
- Cancer cases
- Multiple adhesions
- Large uterus
Comparing Surgical Approaches
Approach | Incision Size | Recovery Time | Hospital Stay | Best For |
Vaginal | None (vagina only) | 2–4 weeks | Outpatient | Simple cases, prolapse |
Laparoscopic | 3–5 small incisions | 2–4 weeks | Same day or overnight | Fibroids, endometriosis |
Robotic | 3–5 small incisions | 2–4 weeks | Same day or overnight | Complex cases, scar tissue, large uterus |
Abdominal | 6–8 inch incision | 4–6 weeks | 2–3 days | Cancer, large or diseased uterus |
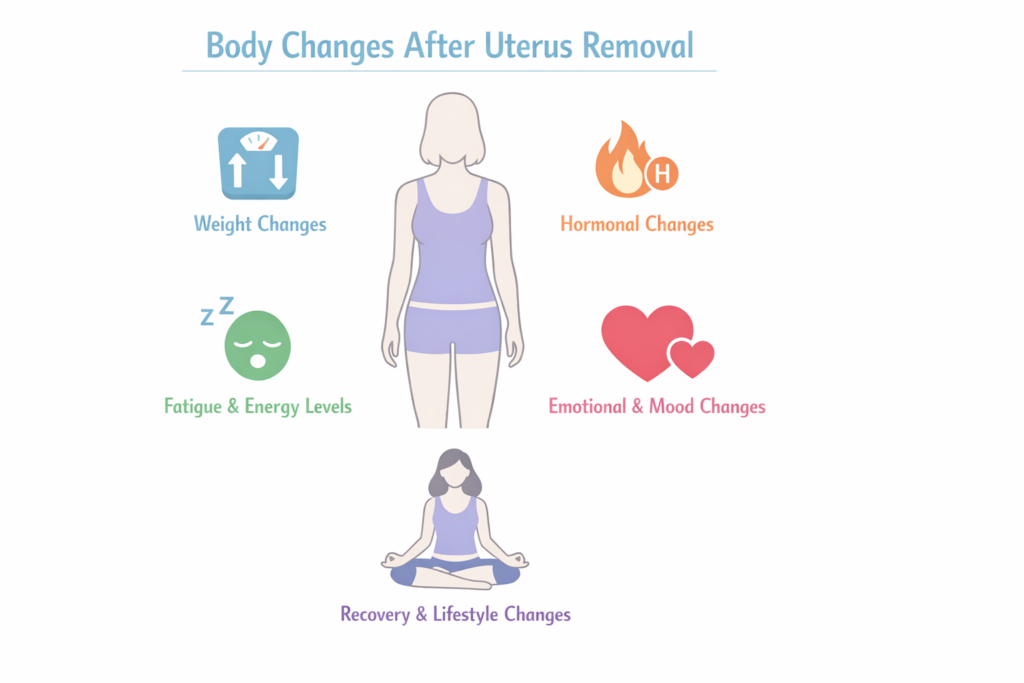
Recovery After a Hysterectomy
General Tips
Avoid heavy lifting (>10 lbs) for 4–6 weeks
Walk daily to prevent blood clots
Follow pain management instructions
Avoid vaginal intercourse for 4–6 weeks
Shower only as instructed; avoid baths/swimming for 6 weeks
Common Side Effects
Vaginal bleeding/discharge (up to 6 weeks)
Soreness or irritation at incision sites
Fatigue or tiredness
Menopause symptoms if ovaries removed: hot flashes, vaginal dryness, low libido
Risks and Complications
Blood clots
Infection
Bleeding
Injury to urinary tract or bowel
Complications from anesthesia
Adhesions or scar tissue
Robotic and minimally invasive approaches generally reduce blood loss, pain, and recovery time compared to open abdominal hysterectomy.
Some patients experience a sense of loss or emotional changes, especially if hysterectomy was done for cancer or fertility reasons. Counseling or support groups can help.
FAQs About Types of Hysterectomy
1️ What is a Type 1 hysterectomy?
A Type 1 hysterectomy, also called a total hysterectomy, involves the removal of the uterus and cervix while leaving the ovaries intact. This procedure is commonly performed for conditions like heavy menstrual bleeding, fibroids, or benign uterine diseases. Because the ovaries remain, menopause does not occur immediately, and hormone production continues normally.
Key points:
- Removes uterus + cervix
- Ovaries remain (no immediate menopause)
- Used for non-cancerous conditions
2️ What is a Type 2 hysterectomy?
A Type 2 hysterectomy is also known as a modified radical hysterectomy. In this procedure, the uterus, cervix, and upper portion of the vagina are removed, along with some surrounding tissues but less extensive than a Type 3 hysterectomy. It is often recommended for early-stage cervical cancer or complex uterine conditions.
Key points:
- Removes uterus, cervix, part of the vagina, surrounding tissue
- Less extensive than radical (Type 3) hysterectomy
- Typically performed for early-stage cancer
3️ What is a Type 3 hysterectomy called?
A Type 3 hysterectomy is commonly referred to as a radical hysterectomy. This is the most extensive form of hysterectomy, typically performed for cervical or uterine cancer. It involves removing:
- Uterus
- Cervix
- Upper vagina
- Surrounding tissues (parametrium)
- Sometimes lymph nodes in the pelvic area
Key points:
- Extensive surgery for cancer treatment
- Longer recovery than Type 1 or Type 2
- May induce menopause if ovaries are removed
4️ Which type of hysterectomy is best?
There is no single “best” type of hysterectomy—it depends on the patient’s condition, age, and treatment goals.
- Type 1 / total hysterectomy: Best for benign conditions like fibroids or heavy bleeding.
- Type 2 / modified radical: Ideal for early-stage cancers needing more tissue removal.
- Type 3 / radical: Reserved for advanced cancers or extensive disease.
Other considerations:
- Minimally invasive methods (laparoscopic, robotic, vaginal) often lead to faster recovery and fewer complications.
- The surgeon’s expertise and patient health also influence the “best” choice.
5️ Do all types of hysterectomy remove the cervix?
No, not all hysterectomies remove the cervix.
- Total hysterectomy (Type 1): removes the cervix.
- Supracervical / subtotal hysterectomy: only the upper part of the uterus is removed; the cervix is left intact.
- Radical hysterectomy (Type 3): removes the cervix along with the uterus and surrounding tissue.
Why it matters:
Keeping the cervix may reduce surgical risks and preserve pelvic support, but it also means Pap tests may still be needed. Removing the cervix eliminates this requirement.