Types of Bariatric Weight Loss Surgery
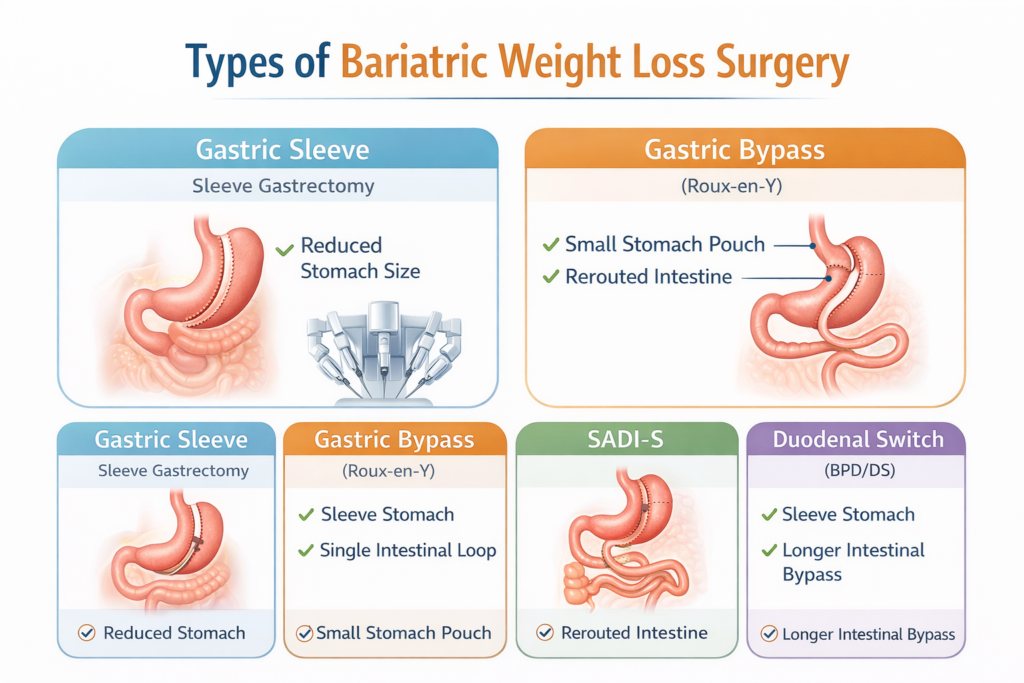
Types of Bariatric Weight Loss Surgery: Complete & Updated Patient Guide
Bariatric surgery, also called metabolic or weight loss surgery, includes a group of medically proven procedures designed to help people with obesity achieve significant and long-term weight loss. These surgeries do more than reduce stomach size they positively change gut hormones, appetite regulation, metabolism, and blood sugar control.
Today, bariatric surgery is one of the most effective treatments for obesity and obesity-related conditions such as type 2 diabetes, high blood pressure, sleep apnea, joint pain, fatty liver disease, and high cholesterol. With modern laparoscopic and robotic techniques, these procedures are safer than ever, with faster recovery and excellent long-term outcomes.
This guide explains all major types of bariatric weight loss surgery, how each works, who it is best for, and the key pros and cons helping you make an informed decision with your surgeon.
What Is Bariatric Weight Loss Surgery?
Bariatric surgery works by:
- Reducing how much food the stomach can hold
- Changing hunger and fullness hormones
- In some procedures, reducing calorie absorption
These changes help patients eat less, feel full sooner, reduce cravings, and maintain sustainable weight loss. Most procedures also lead to rapid improvement in diabetes and metabolic health, often before major weight loss occurs.
Main Types of Bariatric Weight Loss Surgery
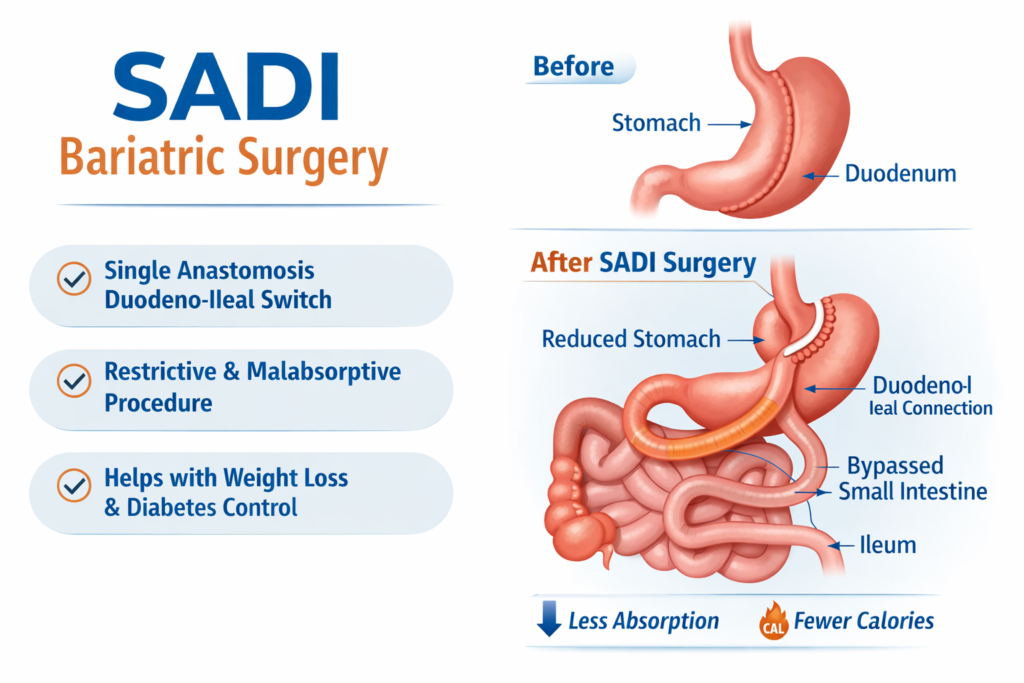
SADI works through three powerful mechanisms:
- Stomach restriction – Smaller stomach means you feel full faster
- Hormonal changes – Reduced hunger hormones and improved insulin sensitivity
- Malabsorption – Shorter intestine length limits calorie and fat absorption
This combination makes SADI highly effective for morbid obesity and type 2 diabetes remission.
Main Types of Bariatric Weight Loss Surgery
The American Society for Metabolic and Bariatric Surgery (ASMBS) recognizes the following procedures as safe and effective when performed at accredited centers.
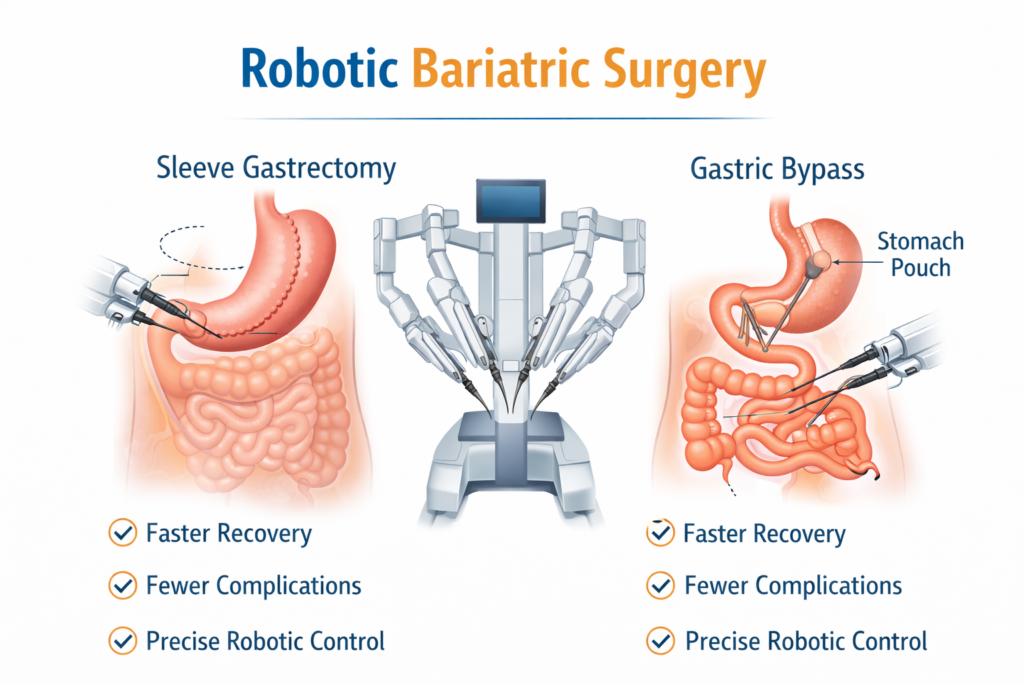
1. Sleeve Gastrectomy (Gastric Sleeve)
Sleeve gastrectomy is the most commonly performed bariatric surgery worldwide.
How the Procedure Works
- About 75–80% of the stomach is permanently removed
- The remaining stomach is shaped like a banana
- No intestinal bypass is done
How It Promotes Weight Loss
- Smaller stomach limits food intake
- Removal of hunger-hormone-producing stomach tissue reduces appetite
- Improves insulin sensitivity and blood sugar control
Advantages
- Simpler and shorter surgery time
- No intestinal rerouting
- Effective weight loss and metabolic improvement
- Often used as a first-stage surgery for high-BMI patients
Disadvantages
- Non-reversible
- May worsen or cause acid reflux in some patients
- Slightly less weight loss than bypass-type procedures
Best for: Patients with moderate to severe obesity seeking a simpler procedure.
2. Roux-en-Y Gastric Bypass
Gastric bypass has been performed for over 50 years and remains one of the most powerful metabolic surgeries.
How the Procedure Works
- A small stomach pouch (egg-sized) is created
- Food bypasses part of the stomach and small intestine
- Digestive juices mix with food further down the intestine
How It Promotes Weight Loss
- Limits food intake
- Reduces calorie absorption
- Strong hormonal changes reduce hunger and improve diabetes
Advantages
- Excellent long-term weight loss
- High remission rates for type 2 diabetes
- Often improves acid reflux
Disadvantages
- More complex surgery
- Lifelong vitamin and mineral supplementation required
- Risk of dumping syndrome
- NSAIDs and smoking must be avoided
Best for: Patients with diabetes, reflux, or severe metabolic disease.
3. Adjustable Gastric Band (Lap-Band)
Adjustable gastric banding is now rarely performed due to lower long-term success.
How the Procedure Works
- A silicone band is placed around the upper stomach
- Creates a small pouch above the band
- Band tightness is adjusted through a skin port
Advantages
- No stomach or intestine removal
- Lowest early complication rate
- Reversible
Disadvantages
- Slower and less weight loss
- High re-operation and removal rates
- Risk of band slippage or erosion
Best for: Selected patients only; largely replaced by other procedures.
4. Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
BPD/DS provides the greatest average weight loss but is also the most complex.
How the Procedure Works
- Sleeve gastrectomy is performed
- Food bypasses about 75% of the small intestine
How It Promotes Weight Loss
- Strong restriction + powerful malabsorption
- Profound hormonal effects on hunger and diabetes
Advantages
- Highest weight loss potential
- Most effective surgery for type 2 diabetes
Disadvantages
- Higher risk of nutritional deficiencies
- Requires strict lifelong follow-up
- More frequent bowel movements
Best for: Patients with very high BMI and severe diabetes.
5. SADI-S (Single Anastomosis Duodeno-Ileal Bypass with Sleeve)
SADI-S is a newer, simplified version of duodenal switch with strong outcomes.
How the Procedure Works
- Sleeve gastrectomy is performed
- One intestinal connection reroutes food
Advantages
- Excellent long-term weight loss
- Strong diabetes remission
- Shorter operative time than DS
Disadvantages
- Newer procedure with limited long-term data
- Risk of vitamin deficiencies
- May worsen reflux
Best for: Patients needing more weight loss after sleeve or with severe metabolic disease.
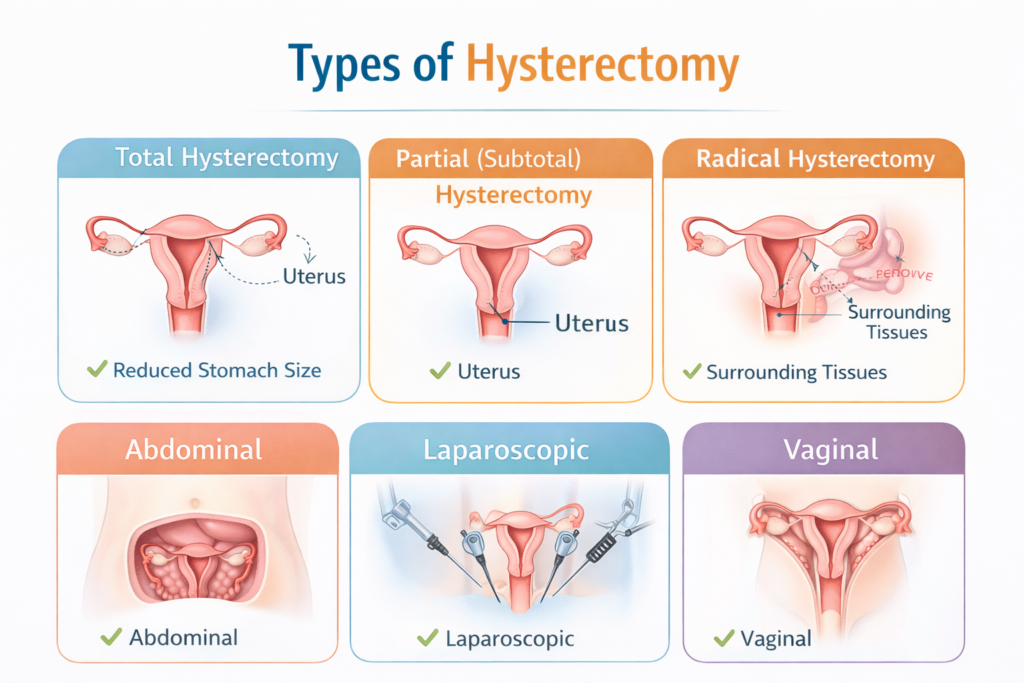
Laparoscopic vs Robotic Bariatric Surgery
Most modern bariatric surgeries are performed using minimally invasive techniques:
- Laparoscopic surgery: Standard approach using small incisions
- Robotic surgery: Surgeon-controlled robotic arms offer greater precision
Robotic bariatric surgery may reduce blood loss, improve accuracy in complex cases, and support faster recovery.
Which Bariatric Surgery Is Best?
There is no single “best” surgery for everyone. The right procedure depends on:
- Body Mass Index (BMI)
- Diabetes severity
- Acid reflux history
- Eating habits
- Previous bariatric surgery
A bariatric surgeon will evaluate your medical history and goals to recommend the safest and most effective option.
Life After Bariatric Surgery
Long-term success requires:
- Healthy eating habits
- Regular physical activity
- Lifelong vitamin supplementation
- Regular medical follow-ups
When combined with lifestyle changes, bariatric surgery can dramatically improve quality of life and life expectancy.
Final Thoughts
Bariatric weight loss surgery is a powerful, evidence-based treatment for obesity and metabolic disease. With multiple surgical options available today, patients can achieve safe, sustainable weight loss and long-term health improvement.
Choosing the right surgery and the right surgical team is the most important step toward success.
FAQs About Types of Bariatric Weight Loss Surgery
1️ What are the three types of bariatric surgery?
Bariatric surgery primarily falls into three categories, each targeting weight loss differently:
- Restrictive Surgery – Reduces stomach size to limit food intake.
- Examples: Sleeve gastrectomy, Adjustable gastric band (lap band)
- Effect: You feel full faster, eat less.
- Examples: Sleeve gastrectomy, Adjustable gastric band (lap band)
- Malabsorptive Surgery – Alters digestion so fewer calories and nutrients are absorbed.
- Examples: Biliopancreatic diversion with duodenal switch (BPD/DS)
- Effect: Promotes significant weight loss, especially for severe obesity.
- Examples: Biliopancreatic diversion with duodenal switch (BPD/DS)
- Combination Surgery – Combines restriction and malabsorption.
- Examples: Roux-en-Y gastric bypass, Single Anastomosis Duodeno-Ileal Bypass with Sleeve (SADI-S)
- Effect: Limits food intake and nutrient absorption, often leading to the most effective long-term weight loss.
- Examples: Roux-en-Y gastric bypass, Single Anastomosis Duodeno-Ileal Bypass with Sleeve (SADI-S)
2️ What is the most successful type of bariatric surgery?
The most successful bariatric surgeries in terms of long-term weight loss and improvement of obesity-related conditions are:
- Roux-en-Y Gastric Bypass (RYGB) – Combines restriction and malabsorption; highly effective for weight loss and diabetes remission.
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS) – Very effective but more complex, usually for severe obesity.
- SADI-S (Single Anastomosis Duodeno-Ileal Bypass with Sleeve) – Newer, simpler version of BPD/DS with excellent results.
Key takeaway: “Success” depends on your health, adherence to diet, and lifestyle changes after surgery.
3️ What foods cannot be eaten after bariatric surgery?
After bariatric surgery, certain foods can cause discomfort, slow weight loss, or damage your stomach. Avoid:
- Sugary and high-fat foods – Can trigger dumping syndrome (nausea, diarrhea, dizziness).
- Carbonated drinks – Cause bloating and discomfort.
- Tough meats or fibrous foods – Hard to digest, may cause blockages.
- Sticky foods – Such as peanut butter or caramel that stick to your pouch/stomach.
- Alcohol – Highly caloric and absorbed faster post-surgery, increasing risks.
Stick to protein-rich, soft, well-cooked foods and small portions for best results.
4️ How long is bariatric surgery?
The duration of bariatric surgery varies depending on the type and surgical method:
- Sleeve gastrectomy: ~60–90 minutes
- Roux-en-Y gastric bypass: ~90–150 minutes
- BPD/DS or SADI-S: ~120–180 minutes
Notes:
- Minimally invasive (laparoscopic or robotic) surgeries may take slightly longer but reduce recovery time.
- Surgeon experience and patient complexity can affect total time.
5️ What is the safest kind of bariatric surgery?
All bariatric surgeries are generally safe when performed at accredited centers, but safety varies by procedure:
- Sleeve gastrectomy – Technically simpler, lower complication rate, widely considered safest overall.
- Adjustable gastric banding – Also low-risk, but long-term weight loss may be less.
- Roux-en-Y gastric bypass – Safe but slightly higher risk due to complexity.
- BPD/DS and SADI-S – Highly effective but involve malabsorption, increasing risk of nutritional deficiencies.