What is Robotic surgery?
- May 16, 2025

Surgical care has evolved dramatically over the past century—from the era of large, invasive incisions and prolonged hospital stays to today’s highly advanced, minimally invasive procedures. What once required open surgery with significant recovery time can now be accomplished through keyhole incisions with unmatched precision, thanks to the advent of robotic-assisted surgery.
In the early days, surgery was often seen as a last resort. The tools were basic, the procedures were lengthy, and outcomes carried considerable risk. The introduction of laparoscopic surgery in the late 20th century marked a major breakthrough. It allowed surgeons to operate using small incisions, guided by cameras and long instruments. This approach reduced pain, minimized complications, and helped patients recover faster. However, even laparoscopy had its limitations—restricted range of motion, reduced visibility, and physical strain on surgeons during long operations.

The next leap forward came with the development of robotic surgical systems—a technological evolution that has redefined what modern surgery can achieve. These systems combine a surgeon’s expertise with the precision of robotic arms, offering three-dimensional high-definition views and a level of control that exceeds the human hand. Robotic surgery enhances safety, accuracy, and outcomes, especially in complex procedures involving the digestive system and internal organs.
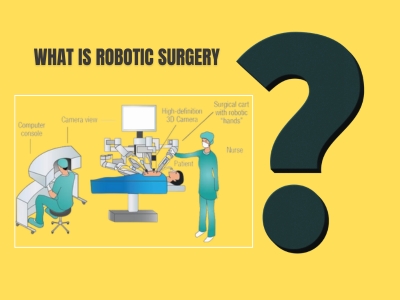
What is Robotic Surgery?
Robotic surgery is a cutting-edge surgical technique that uses computer-assisted robotic systems to perform complex procedures with enhanced precision, flexibility, and control. Unlike traditional open surgery, where a surgeon operates directly with their hands, or even standard laparoscopy which relies on rigid instruments, robotic surgery allows the surgeon to operate from a specialized console, where every movement of their hands is translated into real-time, fine-tuned actions by robotic arms inside the patient’s body.
The most well-known system used globally is the da Vinci Surgical System, which has transformed the landscape of minimally invasive surgery. This system comprises three main components:
- Surgeon Console: Here, the surgeon sits comfortably and views the surgical site in high-definition 3D, magnified up to 10 times. Using master controls and foot pedals, the surgeon manipulates the robotic arms with precision.
- Patient-side Robotic Arms: These robotic arms are attached to tiny instruments and a 3D camera. They mimic the surgeon’s movements with high accuracy and can rotate and bend in ways far beyond the capability of the human wrist.
- Vision System: The robotic system provides a crystal-clear, magnified view of the surgical field, allowing the surgeon to see fine anatomical details and perform delicate manoeuvres with confidence.

Despite its name, the robot does not operate on its own. Every movement and decision is entirely controlled by the surgeon. The robot acts as an extension of the surgeon’s hands, providing enhanced reach, steadiness, and accuracy—especially in tight or delicate areas such as the digestive tract, pelvic cavity, or near vital nerves and blood vessels.
The core components of MASH include:
- Abdominal Obesity: Excess fat around the abdomen is a major risk factor for developing metabolic syndrome. This is typically measured by waist circumference or waist-to-hip ratio.
- Insulin Resistance: When the body’s cells don’t respond properly to insulin, leading to elevated blood sugar levels. Insulin resistance is a precursor to type 2 diabetes.
- High Blood Pressure: Increased blood pressure, also known as hypertension, is another key component. It puts extra strain on the heart and can lead to cardiovascular problems over time.
- Dyslipidemia (Abnormal Cholesterol Levels): This includes high levels of LDL (bad cholesterol), low levels of HDL (good cholesterol), and high triglycerides, which increase the risk of heart disease.
- Elevated Blood Glucose Levels: This is a condition where the blood sugar levels are higher than normal, a precursor to type 2 diabetes.
Application Areas of Robotic Surgery
Robotic surgery has become a cornerstone in the advancement of minimally invasive procedures, especially in the field of abdominal and gastrointestinal health. Its application spans a wide range of complex surgical procedures that benefit from enhanced precision, reduced trauma, and faster recovery. Here are the major areas where robotic surgery is making a significant impact:
1. Advanced Gastrointestinal (GI) Surgeries
The digestive system is a complex network of organs, and operating within it demands extreme precision. Robotic surgery allows for safer, more refined movements, especially in deep or narrow areas such as the pelvis or around the intestines.
- Esophageal surgeries, gastric resections, and intestinal reconstructions benefit from enhanced 3D visualization and steady instrumentation.
- The robotic system is especially useful in cases where patients have scar tissue from previous surgeries, obesity-related anatomical challenges, or complex anatomical variations.
- For example, in treating gastric outlet obstruction or severe GERD, robotic surgery offers a highly accurate and less invasive alternative to traditional approaches.
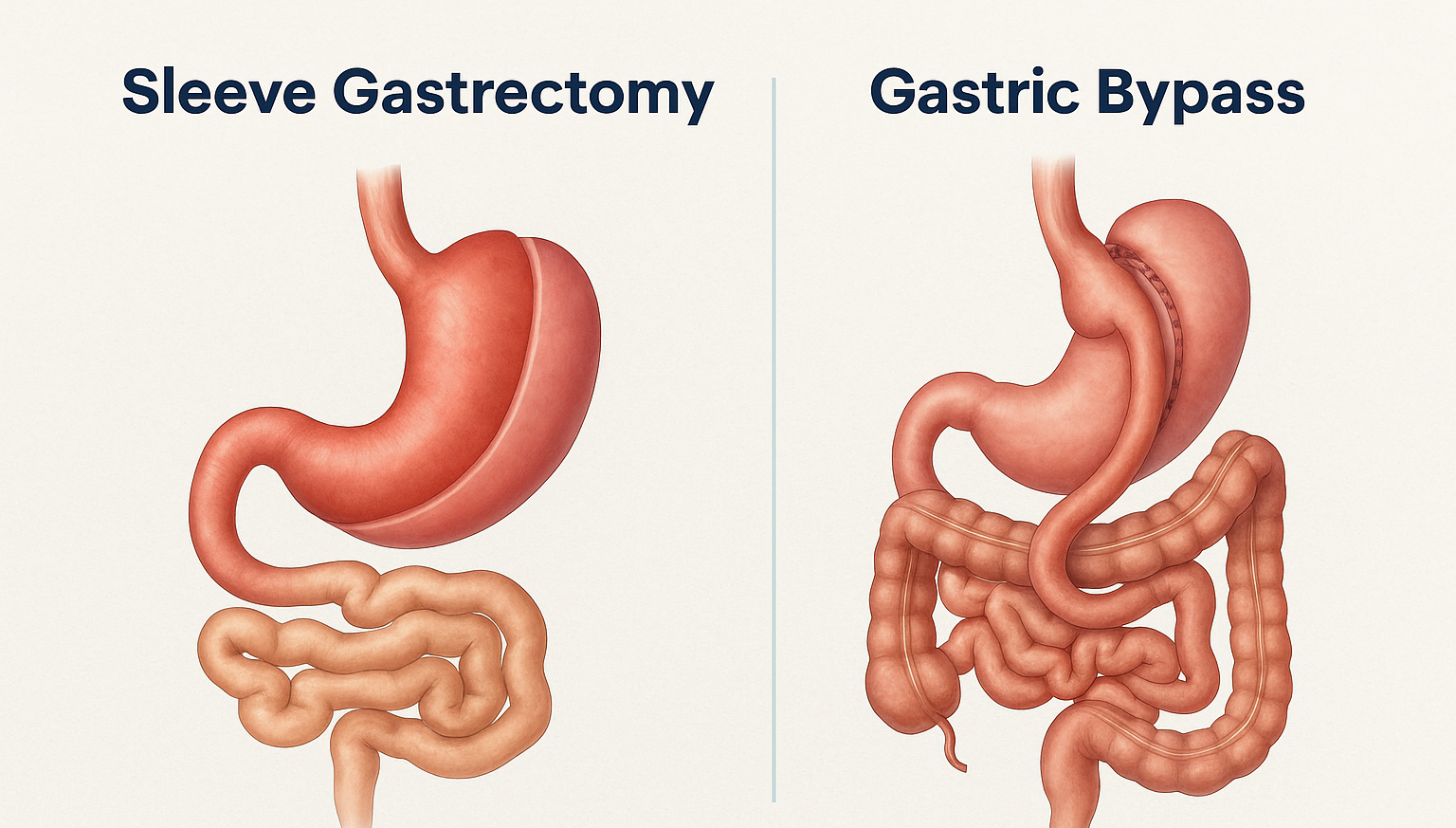
2. Weight Loss (Bariatric) Surgeries
Bariatric procedures are increasingly being performed robotically, especially in patients with higher body mass indexes (BMI) or those requiring revision surgeries.
- Robotic Sleeve Gastrectomy and Roux-en-Y Gastric Bypass are now performed with greater precision and fewer complications.
- The robotic system’s high level of control is particularly useful in morbidly obese patients, where visibility and space are often limited.
- Faster healing, reduced pain, and fewer wound infections make robotic bariatric surgery ideal for patients seeking both safety and effective long-term outcomes.
3. Hernia Repairs
Hernia repair is one of the most common abdominal surgeries, but complex or recurrent hernias—especially those involving mesh, adhesions, or organ entrapment—can be very challenging.
- Robotic-assisted hernia repair allows surgeons to perform intricate tasks such as suturing, mesh placement, and dissection with extraordinary control.
- Patients benefit from lower recurrence rates, less pain, and quicker return to daily activities.
- Particularly for inguinal, ventral, or hiatal hernias, robotic surgery offers enhanced access and durability of repair.
4. Colorectal Surgeries
Diseases of the colon and rectum, such as diverticulitis, inflammatory bowel disease (IBD), and colorectal cancer, often require precise dissection in areas that are difficult to access through traditional surgery.
- Robotic-assisted colectomies, rectal cancer resections, and stricture repairs are now routinely performed with better preservation of nerves, blood vessels, and surrounding organs.
- This is especially beneficial in pelvic surgeries where preserving continence and sexual function is a major concern.
- The robotic system allows for a more complete and safer removal of diseased tissue, particularly in narrow pelvic spaces.
- Robotic assistance allows for more precise removal of diseased segments, better nerve preservation, and improved functional outcomes, particularly in low pelvic areas.
- Robotic colorectal procedures often result in quicker bowel recovery, shorter hospital stays, and fewer complications.
5. Surgical Oncology: Cancers of the Stomach and Intestines
Operating on cancer patients demands the dual goals of complete tumor removal and minimizing damage to surrounding healthy tissue.
- Robotic cancer surgeries in the gastrointestinal tract—such as for gastric cancer, colorectal cancer, and small intestine tumors—enable precise dissection of cancerous tissues while preserving vital structures.
- The high-definition 3D view ensures that no microscopic disease is missed, and the improved dexterity allows for accurate lymph node dissections and anastomoses (joining of tissues).
- For patients who may not be ideal candidates for traditional surgery due to age, prior surgeries, or comorbidities, robotic surgery reduces operative trauma and speeds recovery, enabling quicker transition to additional treatments like chemotherapy or radiation.
- The technology helps in achieving clear margins, reducing intraoperative bleeding, and preserving healthy tissue, which is crucial for postoperative quality of life and effective follow-up treatment.
Benefits of Robotic Surgery
Robotic-assisted surgery offers a wide range of advantages for both patients and surgeons:
For Patients:
- Smaller Incisions: Leads to less scarring and faster healing.
- Reduced Blood Loss: Smaller cuts and more precise movements reduce bleeding.
- Less Pain: Patients often experience less discomfort after the operation.
- Shorter Hospital Stays: Many patients can return home more quickly than after open surgery.
- Faster Recovery Time: Quicker return to normal activities and work.
- Lower Risk of Infection: Smaller wounds reduce exposure to bacteria.
For Surgeons:
- Enhanced Precision: Robotic instruments can move in finer increments than the human hand.
- Better Visualization: High-definition 3D imaging allows for a more detailed view of the surgical site.
- Improved Ergonomics: Surgeons operate from a seated position, which can be less physically demanding during long procedures.
- Tremor Reduction: Robotic systems filter out natural hand tremors, improving accuracy.
Conclusion
Robotic surgery stands at the cutting edge of modern medicine—a symbol of how far surgical care has progressed in just a few decades. It has redefined precision, safety, and recovery in ways that were once considered impossible. From addressing complex gastrointestinal conditions and performing high-risk bariatric procedures to managing intricate hernia repairs and oncological surgeries, robotic-assisted techniques are setting new benchmarks for surgical outcomes worldwide.
The benefits are not just technical. For patients, robotic surgery often means smaller scars, less pain, fewer complications, and a faster return to everyday life. For surgeons, it offers unmatched control, enhanced visibility, and the ability to perform delicate maneuvers with confidence—even in the most challenging cases. It bridges the gap between human skill and technological innovation, making surgeries that were once highly invasive far more manageable and effective.
At the forefront of this medical revolution is Dr. Mufti, whose commitment to excellence, safety, and patient well-being has made him a leader in robotic and minimally invasive surgery. By adopting and mastering these advanced techniques, Dr. Mufti continues to transform the lives of countless patients—particularly those with high-risk profiles or complicated surgical histories. His approach combines cutting-edge technology with deep clinical expertise, ensuring that every patient receives personalized, world-class care tailored to their unique needs.
Robotic surgery is not just the future—it is the present. And with experts like Dr. Mufti leading the way, patients can be assured that they are receiving the very best that modern surgical science has to offer.

© 2025 Copyright : DHI | POWERED BY PEPMEDIA