How Obesity Affects Fertility in Women: What You Need to Know
- May 23, 2025

Fertility is influenced by many factors, but one that often goes overlooked is weight. Obesity can disrupt the body’s delicate hormonal balance, interfere with ovulation, and increase the risk of reproductive disorders. It’s not just a health concern—it’s a fertility issue.
Globally, obesity rates among women have nearly tripled since 1975, with over 15% of women aged 18 and older classified as obese (World Health Organization). In women trying to conceive, a high Body Mass Index (BMI over 30) has been linked to a 50% reduction in the chances of natural conception. Obese women are also more likely to experience irregular menstrual cycles, anovulation (absence of ovulation), and lower success rates with fertility treatments like IVF.
Moreover, conditions such as Polycystic Ovary Syndrome (PCOS)—a leading cause of infertility—are closely tied to excess weight and insulin resistance. Up to 70% of women with PCOS are overweight or obese, creating a cycle that makes conception even more difficult.
This blog explores the science behind how obesity impacts fertility—from hormonal disruptions to PCOS, ovulation issues, and pregnancy complications—along with actionable steps women can take to reclaim control over their reproductive health.
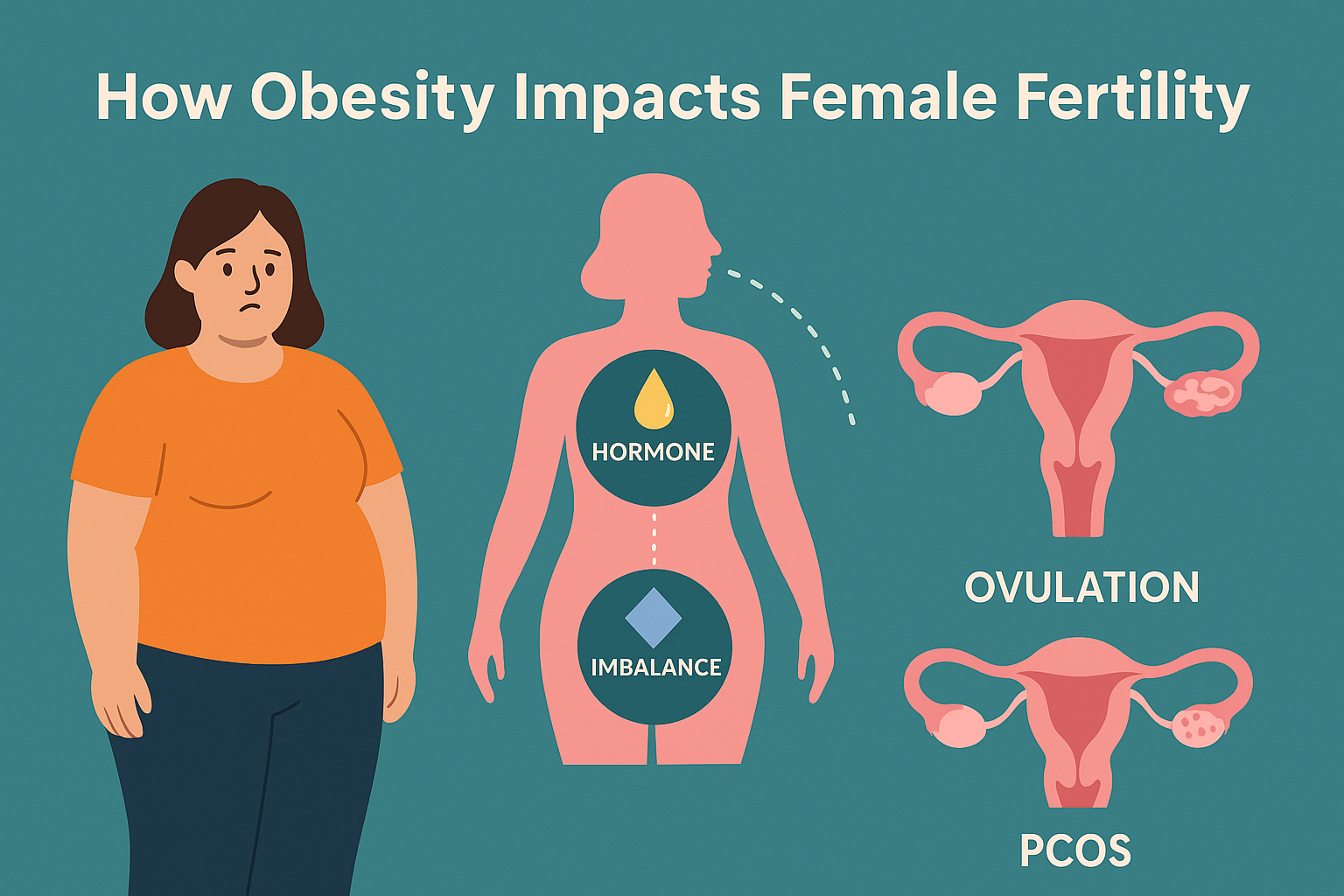
Understanding the Link Between Obesity and Hormones
Fat tissue isn’t just a passive store of energy—it’s hormonally active. It produces estrogen, a crucial hormone for female fertility. However, when estrogen levels are excessively high—as is often the case in women with obesity—the body’s delicate hormonal balance gets disrupted. High estrogen can trick the brain into thinking the body is already ovulating, which suppresses the release of hormones like FSH (follicle-stimulating hormone) and LH (luteinizing hormone)—both essential for egg development and release.
Moreover, obesity often leads to insulin resistance, where the body’s cells don’t respond effectively to insulin. To compensate, the pancreas produces more insulin, but this excess insulin stimulates the ovaries to produce androgens(male hormones such as testosterone). Elevated androgen levels interfere with the maturation of ovarian follicles, leading to poor egg development and lower chances of successful ovulation.
This hormonal chaos ultimately results in irregular cycles, missed periods, and infertility. In short, obesity throws a wrench into the hormonal machinery required for conception.
Ovulation Problems Caused by Obesity
Ovulation—the monthly release of a mature egg from the ovary—is central to a woman’s ability to conceive. In women with obesity, ovulation may become irregular (oligo-ovulation) or may not occur at all (anovulation). This is due to hormonal signals getting misfired or suppressed, which prevents eggs from developing and being released properly.
Even if ovulation does occur, it may be suboptimal, meaning the egg released may not be of good quality or the hormonal environment may not support fertilization and implantation. This results in lower conception rates, increased chances of miscarriage, and reduced pregnancy success.
Many obese women also experience irregular periods, missed cycles, or unusually heavy menstrual bleeding—signs that the ovulation cycle is out of sync. Without predictable ovulation, the window for conception narrows significantly.
PCOS and Obesity: A Complicated Relationship
Polycystic Ovary Syndrome (PCOS) affects nearly 1 in 10 women of reproductive age and is one of the most common causes of infertility. While not all women with PCOS are overweight, a significant majority are—and obesity dramatically worsens PCOS symptoms.
In PCOS, the ovaries produce excess androgens, which leads to symptoms such as:
- Irregular or absent periods
- Multiple small ovarian cysts
- Acne and oily skin
- Excess facial or body hair
- Weight gain and difficulty losing weight
Obesity and insulin resistance create a vicious cycle: excess weight worsens insulin resistance, which then elevates androgen levels, further derailing ovulation. This makes weight loss extremely challenging but also crucial in managing PCOS.
Women with both obesity and PCOS are more likely to suffer from:
- Infrequent or absent ovulation
- Poor egg quality
- Endometrial abnormalities
- Lower success rates with fertility treatments
The good news? Even moderate weight loss can significantly improve symptoms and restore fertility in many women with PCOS.
Impact on Assisted Reproductive Treatments (IVF, IUI)
For women turning to assisted reproductive technologies like IVF (In Vitro Fertilization) or IUI (Intrauterine Insemination), obesity can still be a barrier. Studies show that:
- Obese women often need higher doses of fertility medications
- They may have fewer mature eggs retrieved during IVF
- The implantation and success rates are lower
- There’s a higher risk of early pregnancy loss or miscarriage
Excess body fat can affect the quality of the egg, the uterine environment, and the overall hormonal response to fertility drugs. Additionally, obesity is linked to poorer embryo development, which affects IVF outcomes.
These complications often result in longer treatment durations, more financial strain, and greater emotional stress.
Pregnancy Risks Associated with Obesity
Even after a woman with obesity becomes pregnant, the risks don’t disappear—they shift. Maternal obesity increases the likelihood of numerous pregnancy-related complications, such as:
- Gestational diabetes (high blood sugar during pregnancy)
- Hypertension and preeclampsia (dangerously high blood pressure)
- Preterm labor and miscarriage
- Cesarean delivery and birth trauma
- Stillbirth or neonatal intensive care needs
There are also long-term risks for the baby. Children born to obese mothers may face a higher risk of:
- Childhood obesity
- Type 2 diabetes
- Heart disease and metabolic disorders
Managing weight before conception can significantly reduce these risks and lead to a healthier pregnancy and baby.

Small Changes, Big Impact: Weight Loss and Fertility Recovery
Here’s the most empowering part: you don’t need to lose a massive amount of weight to see benefits. Studies consistently show that losing just 5–10% of body weight can dramatically improve hormone levels, regulate menstrual cycles, and restore natural ovulation.
For example, a woman weighing 90 kg who loses 5–9 kg may start ovulating regularly again—even without medical treatments.
Key lifestyle strategies include:
- Balanced diet: Emphasize whole grains, lean protein, vegetables, and healthy fats
- Regular exercise: Aim for 30 minutes of moderate activity most days of the week
- Better sleep: Poor sleep can worsen insulin resistance and weight gain
- Stress management: High stress can further disrupt hormone balance
In women with PCOS, these changes can improve insulin sensitivity, reduce androgen levels, and restore the body’s natural fertility rhythm.
Taking Charge of Your Fertility Health
Obesity may complicate the journey to parenthood, but it doesn’t make it impossible. Understanding how weight affects your hormones, ovulation, and reproductive health is the first step toward taking control. With even modest weight loss, many women experience more regular cycles, improved ovulation, and a greater chance of natural conception.
By embracing healthier habits—nutritious eating, regular physical activity, quality sleep, and stress management—you’re not just improving fertility, but also setting the foundation for a healthier pregnancy and baby. And if challenges persist, seeking support from a fertility specialist can open doors to personalized treatment and expert guidance.
Your fertility is a vital part of your overall well-being. With awareness, action, and support, you can reclaim it—one small step at a time.

© 2025 Copyright : DHI | POWERED BY PEPMEDIA