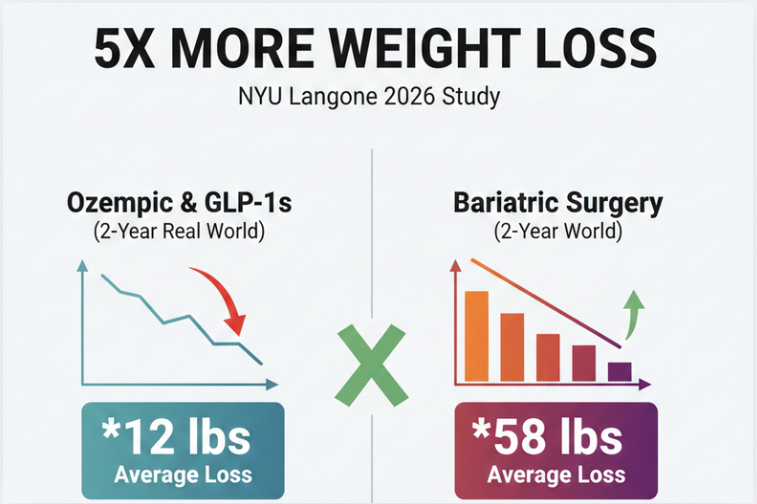
The Weight Loss Option That Beats Ozempic by 5 Times

The Weight Loss Option That Beats Ozempic by 5 Times: Science’s 2026 Update
The honeymoon phase with “the shot” is meeting a reality check. While Ozempic and Wegovy dominated headlines for years, a landmark 2025/2026 real-world study has finally revealed a clear winner for long-term results.
If you are looking for the most effective way to lose weight and keep it off, there is one medical path that consistently beats Ozempic by a staggering 5 times in total weight loss: Bariatric (Metabolic) Surgery.
Walking is one of the most natural and accessible forms of physical activity for adults and older teens. Unlike high-intensity workouts or medical interventions such as bariatric surgery, walking is low-impact, safe, and can be incorporated into daily routines without special equipment.
Evidence shows that regular walking contributes significantly to weight loss, fat reduction, and obesity management. According to the Centers for Disease Control and Prevention (CDC), adults should aim for at least 150 minutes of moderate-intensity physical activity per week, and walking is a practical way to achieve this goal.
The question many people ask is: How many steps per day are needed to see meaningful weight loss? The answer varies depending on factors such as body weight, age, metabolic rate, and diet. This blog provides evidence-based guidance on step goals, walking intensity, and practical tips for long-term weight management.
The Study That Shook the Medical World
Researchers at NYU Langone Health recently presented data from over 51,000 patients. Unlike clinical trials, which are “perfect world” scenarios, this study looked at how people actually lose weight in everyday life over a two-year period.
The numbers were undeniable:
Bariatric Surgery Patients: Lost an average of 58 pounds (24% of total body weight).
Ozempic/GLP-1 Patients: Lost an average of 12 pounds (4.7% of total body weight).
Mathematically, surgery led to 5.1 times more weight loss than the injections. But why is the gap so massive when Ozempic commercials promise 15% or more?
Why "The Scalpel" Still Beats "The Needle" in 2026
1. The Adherence Gap (The 70% Drop-Off)
The biggest weakness of Ozempic is that it only works if you take it. The NYU study found that nearly 70% of patients stop taking their GLP-1 injections within the first year. Whether due to side effects, “food noise” returning, or “Ozempic fatigue,” most people don’t stay on the drug long enough to see the results. Surgery is a one-time “reset” that stays with you 24/7.
2. The Hormonal Reset
Ozempic mimics one hormone (GLP-1) to signal fullness. Surgery, however, physically removes the part of the stomach that produces Ghrelin (the “hunger hormone“). By muting the hunger signal at its source, surgery provides a permanent metabolic shift that a weekly shot struggle to match in a real-world setting.
3. The Rebound Effect
In 2026, we are seeing a wave of “rebound” cases. Data shows that when a patient stops taking a GLP-1 drug, the weight often returns within months. Surgery offers a “durable” result; 10-year follow-ups show that surgery patients typically maintain 25% of their weight loss for a decade or more.
2026 Comparison: Surgery vs. Medication
| Feature | GLP-1 Injections (Ozempic) | Metabolic Surgery (Sleeve/Bypass) |
| Real-World Weight Loss | ~5% Average | ~25% Average |
| Commitment | Weekly for life | One-time procedure |
| Hormonal Impact | Temporary suppression | Permanent reset (Ghrelin) |
| Diabetes Remission | High, while on drug | Highest (often within days) |
| Invasiveness | Non-surgical | Minimally invasive |
Is Bariatric Surgery Right for You?
While surgery is the “5x” champion, it is a major medical decision. In 2026, the medical community recommends surgery for:
BMI over 35: Regardless of other health issues.
BMI over 30: If you have metabolic diseases like Type 2 Diabetes or sleep apnea.
GLP-1 Non-Responders: Those who didn’t reach their goals or couldn’t handle the nausea of Ozempic.
The "Hybrid" Trend of 2026
Interestingly, many doctors are now using both. They use drugs like Ozempic to help a patient lose 10% of their weight before surgery to make the procedure safer, or after surgery to help break a plateau.
FAQs About The Weight Loss Option That Beats Ozempic by 5 Times
1. Is bariatric surgery safer than taking Ozempic?
In 2026, bariatric surgery is performed laparoscopically and is considered as safe as gallbladder surgery. While Ozempic is non-invasive, it can cause “stomach paralysis” (gastroparesis) in some users. Both have risks, but surgery is a “one-and-done” risk versus a lifetime of drug side effects.
2. Why did I hear Ozempic causes 20% weight loss?
That 20% number comes from clinical trials where patients are monitored perfectly. In the real world (where people miss doses or struggle with nausea), the average loss is closer to 5%, according to the latest 2025/2026 data.
3. Can I get surgery if I am already on Ozempic?
Yes. Many surgeons actually recommend staying on the medication up until a few weeks before your surgery to improve your metabolic health.
4. What about the new drugs like Retatrutide?
Retatrutide is the “triple-agonist” drug entering the market in late 2026. While it promises higher weight loss than Ozempic, we don’t have real-world data yet to see if people will stay on it long-term. Currently, surgery remains the gold standard for volume and durability.
5. Does the weight come back after surgery?
Approximately 80% of surgery patients maintain significant weight loss for over 10 years. While some “weight creep” can happen, it is rarely as severe as the weight regain seen when someone stops taking weight loss injections.