Am I eligible for bariatric surgery?

In an age where obesity has become a global health epidemic, many individuals find themselves struggling to lose weight despite countless attempts at dieting and exercise. For those facing severe obesity or obesity-related health issues, bariatric surgery presents a potential solution to help manage weight and improve overall health. However, bariatric surgery is not a one-size-fits-all treatment, and eligibility is determined based on various factors including body mass index (BMI), medical history, and psychological readiness.
Bariatric surgery can offer life-changing results for people with severe obesity (BMI ≥ 40) or those who have struggled to manage obesity-related health conditions like type 2 diabetes, sleep apnea, and heart disease. But it’s not an automatic decision. The path to bariatric surgery is a complex one, involving comprehensive medical evaluations and lifestyle assessments to ensure that the individual is physically and mentally prepared for the challenges that come with such a major procedure.
This guide will take you through the eligibility criteria for bariatric surgery, helping you understand the key factors that determine if this treatment is right for you. From BMI thresholds and health conditions to psychological readiness and lifestyle commitment, you’ll gain insight into the factors that influence whether you are a candidate for bariatric surgery.
Understanding Bariatric Surgery
Bariatric surgery is a term used to describe a range of surgical procedures designed to help individuals with severe obesity lose weight and improve their overall health. These surgeries are typically recommended for those who have not been successful in losing weight through traditional methods like diet and exercise and who suffer from obesity-related health issues. The primary goal of bariatric surgery is to alter the digestive system in a way that limits food intake, reduces nutrient absorption, or both, leading to significant weight loss.
There are several types of bariatric surgeries, each with its own approach to helping patients lose weight. Here are the most common procedures:
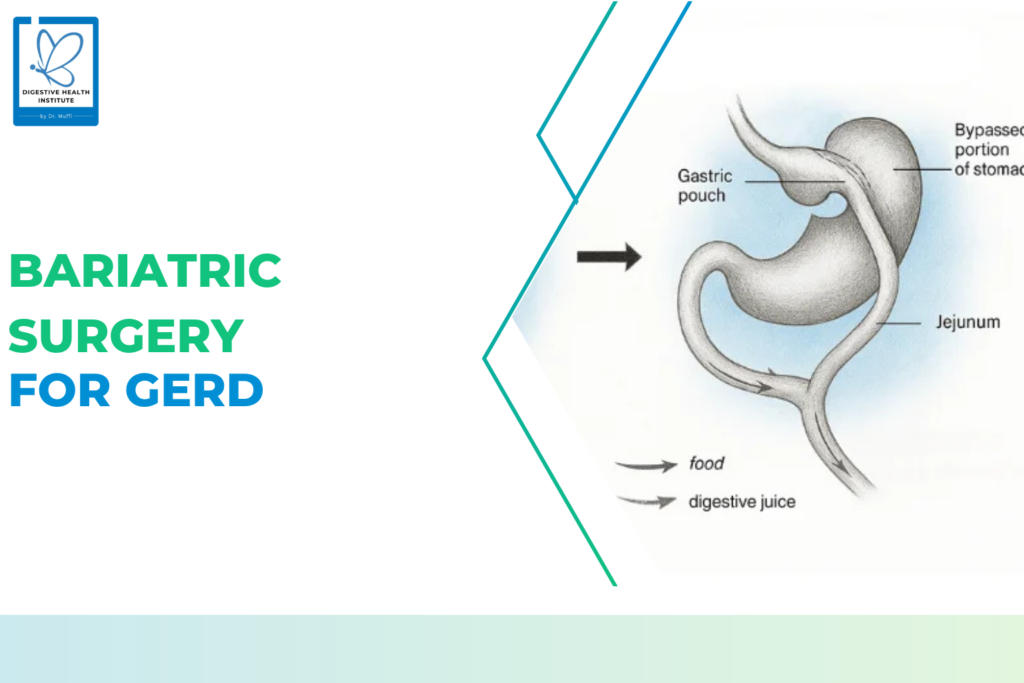
1. Gastric Bypass (Roux-en-Y)
Gastric bypass surgery creates a small stomach pouch and connects it directly to the small intestine, bypassing part of the stomach and the duodenum (the first part of the intestine). This limits the amount of food you can eat and reduces nutrient absorption, leading to weight loss. It can also help manage conditions like type 2 diabetes.
2. Sleeve Gastrectomy
In sleeve gastrectomy, a large portion of the stomach is removed, leaving a tube-shaped stomach about the size of a banana. This reduces the amount of food you can eat and lowers hunger-related hormones, helping control appetite. Unlike gastric bypass, it doesn’t alter the intestines, so there’s less risk of nutrient deficiencies.
3. Adjustable Gastric Banding
This procedure involves placing an adjustable band around the upper stomach to create a small pouch. The band restricts the amount of food the stomach can hold and slows digestion. While less invasive, it is less commonly used today due to the rise of more effective surgeries. Some patients also face challenges with the band.
4. Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
BPD/DS combines stomach reduction with rerouting the intestines, significantly limiting food intake and calorie absorption. This leads to substantial weight loss and helps manage diabetes. However, it’s a more complex surgery and carries higher risks, requiring lifelong follow-up for nutrient management.
You may be eligible if:
1. Body Mass Index (BMI)
Bariatric surgery is typically recommended for individuals with a BMI of:
- 30 or higher with comorbidities like type 2 diabetes, hypertension, or sleep apnea.
- 35 or higher (even without comorbidities) or in cases where traditional weight loss methods have failed.
- A BMI of 40 or higher qualifies most candidates for bariatric surgery.
If you’re in the 30-34.9 range, bariatric surgery might be considered, but it depends on your medical history, lifestyle, and specific health conditions.
It’s important to note that BMI isn’t a perfect metric. Some individuals may have a high BMI due to muscle mass, while others may carry visceral fat that increases health risks. Hence, metabolic assessmentsandwaist-to-hip ratios are also considered in some evaluations.
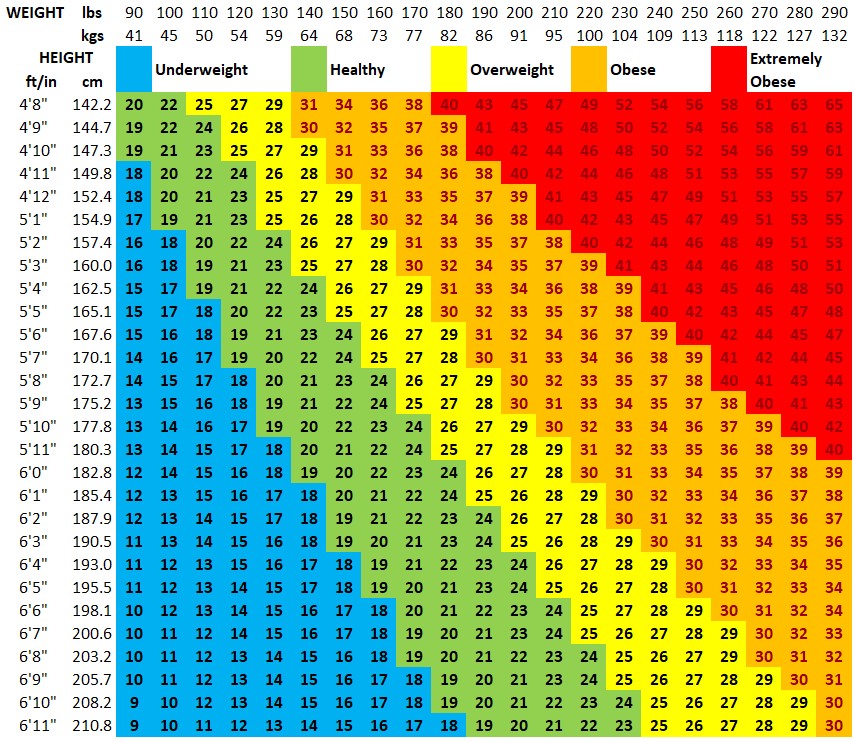
How to view your BMI from the Chart
To view where your BMI lies in this chart, you can first find your weight on the top horizontal axis and then following the BMI numbers all the way down until the height on the left axis corresponds to your height. The category that your body mass index (BMI) lies under is shaded in the corresponding colour which is shown in the legend above as well list below:
- Blue: The category is Underweight and corresponds to a BMI of less than 18.5
- Green: The category is Normal Weight and corresponds to a BMI between 18.5 and 24.9
- Yellow: The category is Overweight and corresponds to a BMI between 25 and 29.9
- Orange: The category is Obese and corresponds to a BMI between 30 and 39.9
- Red: The category is Extremely Obese and corresponds to a BMI of 40 or higher
2. Health Conditions (Comorbidities)
The presence of certain health conditions may make you more eligible for surgery, including:
- Type 2 diabetes
- High blood pressure
- Obesity-related heart disease
- Sleep apnea
- Fatty liver disease or joint issues
If you suffer from any of these, surgery could help manage or even reverse some conditions.
3. Previous Weight Loss Attempts
Bariatric surgery is generally a last-resort option after trying dieting, exercise, and other medically supervised weight loss programs for a significant period (usually 6–12 months).
4. Psychological and Emotional Readiness
Mental health is a vital part of surgical success. That’s why a psychological evaluation is mandatory.
What they Look For:
- Ability to commit to post-surgery lifestyle changes
- Understanding of the procedure and its risks
- Absence of untreated psychiatric conditions (like severe depression or schizophrenia)
- No current substance abuse or eating disorders (e.g., binge eating)
This ensures you’re emotionally equipped to handle the changes that follow—both physically and mentally.
5. Age Range
The general age range for bariatric surgery candidates is between 18 and 65. However, some younger or older individuals may still qualify if deemed fit after a thorough medical assessment.
6. Physical Health
You should be in generally good physical health and able to handle surgery. Doctors will assess any cardiac issues, nutrient deficiencies, or other pre-existing conditions that might pose a risk.
7. Lifestyle Commitment: It Doesn’t End With Surgery
Bariatric surgery is the beginning of a lifelong journey. You must commit to:
- Nutritional changes: Smaller meals, no sugar-sweetened beverages, high-protein diets
- Regular physical activity: 15–30 minutes per day is typically recommended
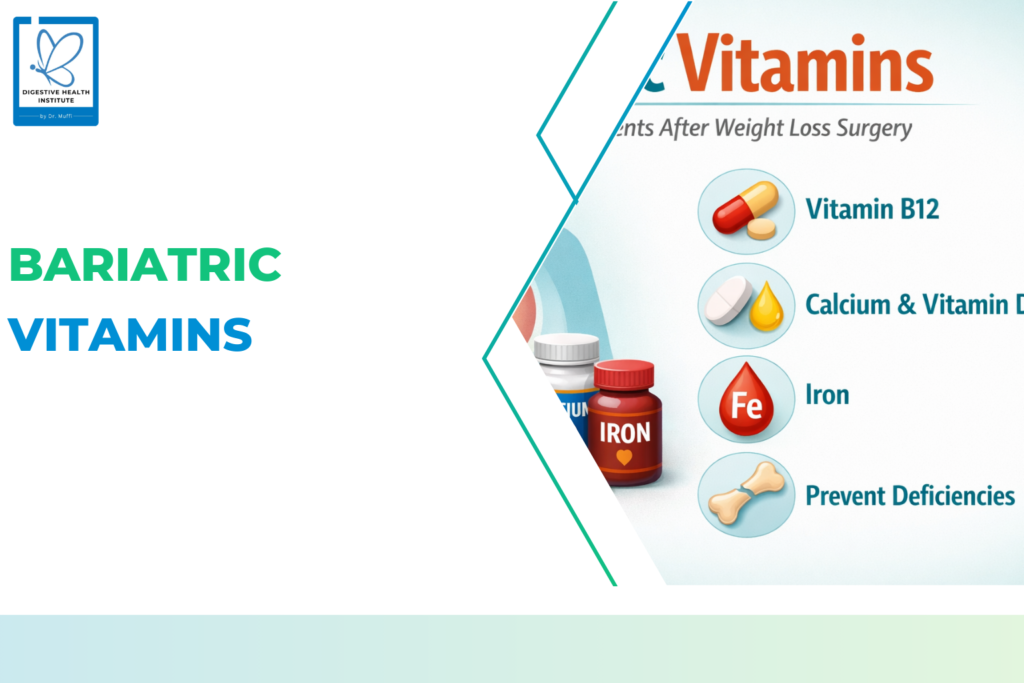
- Vitamin and mineral supplementation: Especially for gastric bypass or duodenal switch patients
- Routine follow-ups: With your bariatric team, dietitians, and sometimes psychologists
Conclusion:
Bariatric surgery can offer life-changing benefits for individuals struggling with severe obesity, especially when traditional methods of weight loss have proven ineffective. However, it’s not a decision to be made lightly. Eligibility for bariatric surgery depends on several factors, including your BMI, the presence of obesity-related health conditions, your previous weight loss efforts, and your emotional and psychological readiness for the lifestyle changes that come with surgery.
It is crucial to have a thorough medical evaluation and to consult with a bariatric surgeon to understand the risks, benefits, and long-term commitments associated with the procedure. Institutions like Digestive Health Institute (DHI), led by Dr. Muffi, offer specialized expertise in evaluating and treating obesity, ensuring that individuals receive the most comprehensive care tailored to their needs.
While bariatric surgery can lead to significant weight loss and improvement in health, success depends on maintaining a healthy lifestyle after surgery, including dietary changes, regular physical activity, and ongoing medical care. Ultimately, bariatric surgery can be an effective tool in your weight loss journey, but it should be approached with careful consideration, preparation, and professional guidance from institutions like DHI to ensure the best possible outcome.